Written by Jacqueline Fitzpatrick
Our sweet Rory was born June 1, 2015, a wonderful surprise at 34 weeks. My first baby, Colin was born in 2013 at 37 weeks after I was induced due to symptoms of HELLP Syndrome. I wasn’t overly concerned when I spontaneously went into labor on May 31, 2015 because I know that Boston has amazing hospitals, 34 weeks isn’t terribly early and I am also an RN making me a bit more comfortable and knowledgeable with the expert medical care in my immediate future. However, what I wasn’t prepared for was the emotional plummet that was going to overcome my entire being a few days later.

Rory’s birth was quick and the neonatal team of RN’s and Neonatologists were in my delivery room when Rory was delivered at 5 pounds 1 ounce. He was immediately surrounded under the heat lamp and with what seemed like a few seconds he was cleaned, hooked up to O2 and Ambu-bagged because he was in respiratory distress. The Neonatologist wrapped him up and let me hold him for exactly 7 seconds. He was then whisked upstairs to the Special Care Nursery (SCN). The next morning I was able to visit him. He looked peaceful on his belly even though he had tubes in his mouth and nose, and leads on his chest and toes. The tube placed in his mouth was to help relieve air from his stomach. That tube was removed a day later and replaced with a tube in his nose, a nasogastric tube (NG tube) for tube feeds of my breast milk. As I sat in my wheel chair holding my sweet boy longer than 7 seconds I felt an overwhelming feeling of mother baby connection. It didn’t register that he would not be coming home with me the next day as I was still recovering from delivery and enjoying just being present.

The next day, discharge day for me, was the beginning of deep feelings I never knew I could get to. The anxiety, guilt and eventual depression began to settle in and little did I know, these feelings would last for 8 months and worsen.

The Neonatologist projected about a 7 day stay for Rory to allow for his lungs to continue maturing. Apnea spells (a pause in breathing that lasts longer than 20 seconds, causing a decrease in blood oxygen levels) is a common occurrence in premature infants and Rory was frequently spelling. Once he was able to be “spell free” for five straight days he would be able to be discharged. Knowing that I had to leave at some point that day I started to get anxious. I was battling between wanting to get this experience of me leaving without my infant over with, feeling sick about leaving my infant behind and longing to see my two year old at home who was wondering where his mama has been. It was time. I made my way to my post partum room and packed my bag. I sat on the end of the hospital bed and sobbed alone. Who doesn’t take their baby home with them? I sobbed some more. I was self conscious of the nurses seeing me in this state and quickly got myself together and thought “Why am I having a pity party? My son is being cared for beautifully by professionals.” I left the hospital with my husband, Shaun, and fully embraced my sweet two year old, Colin at home.
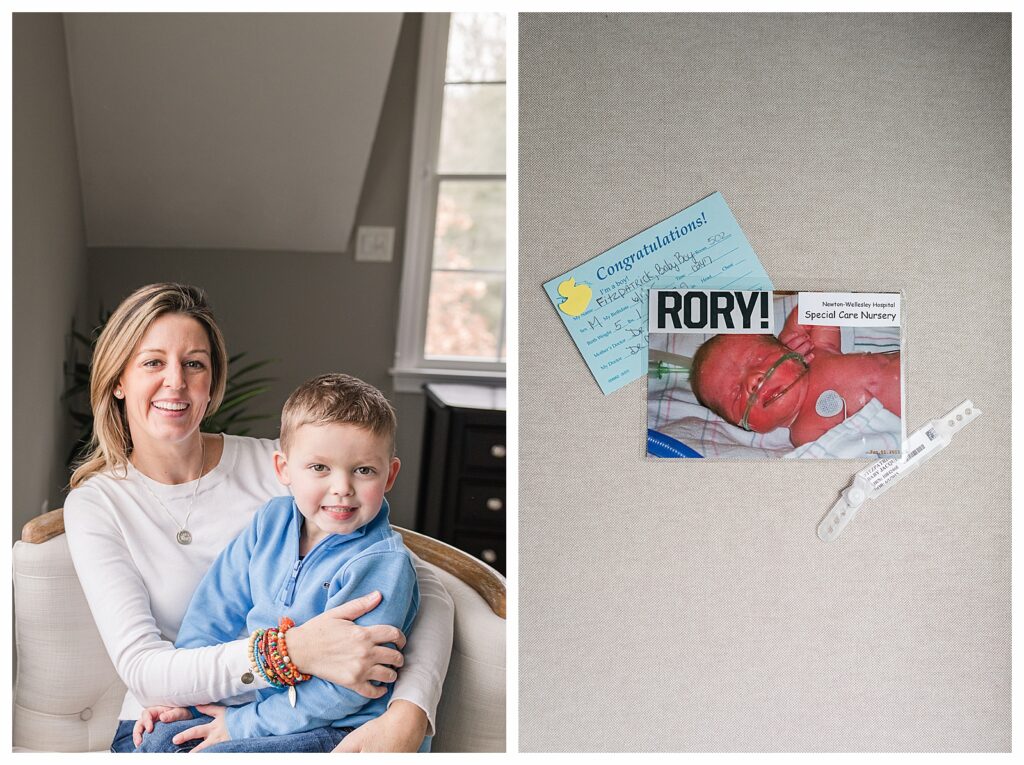
My new routine would look like this: Sleep through the night with one wake to pump, call the SCN each morning at 7:30 am and find out Rory’s feeding schedule for the day. He would eat every 3 hours via NG tube of my milk that I pumped and brought to the hospital to store. Knowing that I had a toddler at home the RN’s suggested that I find one or two feeding times for the day to be in the hospital with Rory to try nursing him and provide skin to skin time. Think about it, I was in the hospital for 4 hours max out of 24 hours to be with my newborn. I was frantically finding childcare for Colin and I could tell he was confused with all of his displacement. The guilt of leaving Colin to rush in for a feedings and the guilt of saying good bye to Rory until the next day took a toll on me. Shaun would visit Rory each evening after work and send me videos of them saying goodnight to me. It was the best. This was our routine for 36 days. Rory stayed well past the projected 7 days because he was continuing to have apnea spells. I would witness Rory’s monitor alarming, meaning that his oxygen levels were decreasing; the nurses don’t rush in as the babies can typically start breathing again on their own. However, 20 seconds is a long time to sit and watch your baby have oxygen desaturation. Occasionally, he would start to turn a bit bluish, but it still wasn’t 20 seconds. We would give Rory a little nudge and he would start breathing on his own, begin turning pink again and the alarm would silent. The SCN became my 2nd home for over a month. I buzzed in each morning, washed my hands, said hello to all the RNs and MDs that had gotten to know me as a “regular” and hear all the stories of which RN was fighting over caring for Rory each day. We joked that Rory became the “Mayor” of the SCN as he stayed the longest so far that summer. Being a second time mother the RNs would leave me alone to be with Rory and provide him with all of his routine care. Just the two of us were behind a purple curtain spending the most quality time, I am sure, I will ever spend with him. Our routine, although chaotic at times became comfortable and I loved pulling into the hospital parking lot, giddy to see and smell my sweet boy. The RNs provided special touches for parents/infants during our stay. Shaun received a Father’s Day card from Rory with his two tiny footprints inside the card. They would post signs up in each infant’s bay when they hit certain goals and provided them with handmade blankets from hospital volunteers. The staff was our biggest cheerleaders! He was discharged on July 7th, 2015. He arrived home with an Oxygen monitor and oral caffeine to keep his brain alert until his scheduled sleep study that would confirm he was no longer apneic and able to discontinue the caffeine.

Teaching and information prior to a SCN stay isn’t typically provided to the expectant mother because it’s usually an unexpected event. Given that, I wish the hospital had social workers more available to prepare us for departing the hospital without the baby, signs of anxiety and depression following and how to manage a schedule with a working spouse and other children in the home. Many spouses are not able to take time off due to unexpected early arrivals and potential baby hospital stays, which was the case in my personal life. I had to handle a lot on my own during the day, which was too much. My experience with the RN’s and neonatologists in the SCN was amazing. I thought I would be visiting Rory daily and delivering my milk supply, but they made life more organized for my already chaotic brain.

Any parent who may experience the SCN my advice to you would be to ask as many questions as possible about how to handle a daily routine for visiting. They may give you times that are better to be with your baby. Call the SCN floor anytime you want. There were a few times early on that I would wake up at 2: am and have an overwhelming urge to call and check in on Rory. Don’t feel guilty that you’re not there 24 hours a day. At the beginning, I had self deprecating guilt, which morphed into paranoia that I was being judged by the staff that I wasn’t there all day. I got over it by opening up to the RN’s about my feelings and they quickly chuckled and told me that I was lucky to be able to come in at all. This startled me; however, there are so many different socioeconomic backgrounds that arrive through the doors of the SCN and many who live a long enough distance away that it is difficult to visit daily. One other piece of advice I would give is to the spouses and family members to make sure they keep an eye on “mom’s” well being. I personally, fell into a deep post-partum depression after pushing through and being strong for my newborn and toddler and family needs. I suffered for 8 months as it worsened and was finally medicated with anti-depressants that changed my life for the better. My SCN experience has made me a stronger human. Thank goodness for the RN’s and MD’s who dedicate their time to help our newborns strive.

BE THE FIRST TO COMMENT